What is Ulcerative Colitis?
Ulcerative Colitis is an autoimmune disease that primarily affects the distal (final) part of the large intestine (colon), progresses towards upper segments over time, involves chronic inflammation of the mucosa layer lining the inner surface of the colon, follows a course with periods of flare-ups and remissions, and causes ulcer formation on the mucosal surface.
What does Autoimmune Disease mean?
AUTOIMMUNE disease is the general term used for all diseases that arise as a result of our body’s defense system chronically attacking and destroying our own tissues and organs due to impaired perception caused by many reasons, perceiving our own tissues as foreign and/or harmful.
Autoimmunity is a case of mistaken identity. The immune system reacts to its own tissues and cells as if they were pathogens.
What are the most well-known autoimmune diseases?
- Ulcerative Colitis
- Crohn’s Disease
- Allergic Asthma
- Rheumatoid Arthritis
- Systemic Lupus
- Autoimmune Vasculitis (Behçet’s Disease, etc.)
- Multiple Sclerosis
- Type 1 Diabetes
- Etc.
Why are Autoimmune Diseases important?
If the process that initiates autoimmunity does not stop or cannot be stopped, each autoimmune disease that develops facilitates the formation of other autoimmune diseases. It is possible to call this an autoimmune storm.
Worldwide, in the last 50 years, while treatable infectious diseases have rapidly decreased, AUTOIMMUNE diseases have been increasing like an avalanche and continue to increase.
Who is most commonly affected by Ulcerative Colitis?
The worldwide annual incidence rate of Ulcerative Colitis is reported as 10-12 per 100,000.
No significant predisposition has been identified between men and women.
The frequency of occurrence increases in industrialized societies.
Genetics is an important factor. In those with first-degree relatives with Ulcerative Colitis, the risk increases to approximately 10-12 times that of the normal population, and this becomes approximately 95 times in identical twins.
Industrial nutrition is another factor that increases risk. While the risk increases in those who eat intensively with meat and dairy products, vegetable-based nutrition reduces the risk.
Intensive antibiotic use and chemotherapy application are among the factors that increase risk.
It is known that the risk of developing Ulcerative Colitis in the following year increases 8-10 times in those who have had Salmonella or Campylobacter infection.
The risk is higher in those with any autoimmune disease.
What are the symptoms of Ulcerative Colitis?
- Bloody Bowel Movements
- Mucous (Slimy) Bowel Movements
- Abdominal Pain
- Diarrhea
- Increased Number of Bowel Movements
- Tenesmus (continuous feeling of needing to defecate)
- Weight Loss
- Nocturnal Bowel Movements
- Chronic Fatigue
- Sleep Disorders
- Depression
- Sexual Dysfunction
How is Ulcerative Colitis diagnosed?
In the diagnosis of Ulcerative Colitis, general examination considering clinical findings first is extremely valuable. Apart from examination, the most valuable diagnostic tool that leads us to diagnosis is endoscopic examination performed by an experienced physician. This endoscopic examination is often sufficient for diagnosis, but biopsy taken from the colon mucosa for pathological examination is important.
Increased erythrocyte sedimentation rate and elevated CRP values in blood tests support the diagnosis.
Elevated Calprotectin and Zonulin in stool examination also support the diagnosis of Ulcerative Colitis.
What is the basic pathology in Ulcerative Colitis?
It is the initiation of chronic autoimmune process due to the loss of biodiversity of the digestive system microbiota (especially colon microbiota) and the weakening of factors protective of the colon mucosa.
The critical threshold here is digestive system MICROBIOTA damage.
What does Digestive System MICROBIOTA mean?
The collection of various microorganisms living in the digestive system is collectively called intestinal MICROBIOTA and deeply affects many aspects of host physiology including nutrient metabolism, resistance to infection, and immune system development.
Trillions of microorganisms that make up the MICROBIOTA live on mucosal membranes (inner skin) covering the digestive system, maintaining a symbiotic (mutually beneficial) relationship with the host’s immune system.
Intestinal bacteria ferment indigestible carbohydrates to produce short-chain fatty acids (SCFAs) such as acetate, propionate, and butyrate. These SCFAs act as biologically active compounds and provide energy for colon epithelial cells. Particularly butyrate serves as the primary energy source for colon epithelial cells. Since microbiota damage will harm SCFA production, the colon epithelium loses serious support.
POSTBIOTIC
There are biologically active components called postbiotics, mainly secreted by bacteria. Among postbiotics, structures called surface layer proteins (SLP) form the first contact line with colon contents in the colon mucosa. SLP is a component of the mucous secretion called mucus that covers the entire digestive system mucosa.
The decrease in biodiversity of MICROBIOTA and its change in favor of pathogens affects active mucus formation and SLP formation, making the colon mucosa vulnerable to external influences. This process is the most important stage in the formation of Ulcerative Colitis.
How is Ulcerative Colitis treated?
The targeted purpose in current Ulcerative Colitis treatment is to suppress the flare-up periods of the disease, prevent flare-ups from occurring, and/or provide milder and shorter flare-up periods.
Ulcerative Colitis is a disease that shows attack (flare-up) and remission periods. The frequency and duration of attack and remission periods are extremely variable from person to person, because there are hundreds of underlying factors causing this variability. Even in the same person, it tends to show a fluctuating course over time.
The main drugs used in Ulcerative Colitis treatment are; 5-aminosalicylic acid, corticosteroid, azathioprine, etc.
In all these treatments, the disease is not completely cured, only suppressed.
By eliminating the factors that initiate or trigger the pathophysiological process of disease formation, cause damage to the colon mucosa, and initiate the autoimmune process, both autoimmune processes can be regressed and Ulcerative Colitis can be treated. What needs to be done for this is to restore the damaged colon MICROBIOTA. Colon microbiota restoration can be done with Fecal Microbiota Transplantation (FMT) or Total Gastrointestinal Flora Transplantation (TGFT), which is a more specific microbiota restoration model. The purpose of FMT and TGFT treatment is to re-establish healthy and highly biodiverse microbiota.
What is Fecal Microbiota Transplantation (FMT)?
FECAL TRANSPLANTATION is the method of endoscopically transferring FMT transplant material obtained after processing fresh feces (stool taken at most 30 minutes before transplantation) from donor candidate(s) who meet healthy donor criteria (Tables 1 and 2) through certain processes to the large intestine of the patient.
The more donors the FMT material is prepared from, the more effective the FMT treatment will be.
FMT is applied at least once. However, the ideal for FMT is to apply a total of 5 sessions with 5-7 day intervals.
FMT is applied endoscopically in the hospital, under operating room conditions, under sedation/general anesthesia.
At least 400 grams of fresh feces must be used in each FMT session.
The patient can be discharged 2 hours after FMT application and can travel on the same day.
The patient can start eating 2 hours after FMT application.
The donor does not need to be of the same gender and nationality as the patient, nor does it need to be a genetic relative.
What is FLORA TRANSPLANTATION (Total Gastrointestinal Flora Transplantation: TGFT)?
It is the process of transferring flora transplant materials taken from donor candidate(s) who meet healthy donor criteria (Tables 1 and 2), under general anesthesia, endoscopically and colonoscopically, from approximately 40-45 different anatomical areas, after being processed through certain procedures, to the patient under general anesthesia, to the equivalent area of the region from which it was taken by endoscopic and colonoscopic method.
A single session of TGFT is sufficient.
After TGFT, donors can be discharged after 8 hours. Patients are discharged one day after TGFT is performed. After discharge, both donor and patient can travel on the same day. Patients start eating 4 hours after TGFT. Donor candidates can start eating 2 hours after the procedure.
As long as no extraordinary developments occur in patients who undergo TGFT, the transplant performed is permanent for life.
Since microbiota samples taken from 45 different regions in TGFT are transplanted to equivalent regions, it is a regionally specific procedure. However, there is no regional specificity in FMT.
The purpose of performing TGFT is to restore the entire digestive system flora (microbiota) from mouth to anus. FMT is aimed only at restoring colon flora (microbiota).
What is the purpose of performing FMT and TGFT?
The aim is curative treatment. However, even if this cannot be achieved, it is important to alleviate symptoms during attack periods, shorten attack durations, and reduce attack frequency.
Frequent defecation and continuous feeling of need to defecate (tenesmus) cause social isolation in patients, they cannot go very far from home or workplace, and especially cannot use long-term public transportation. With FMT or TGFT to be performed, the daily number of defecations will decrease and diarrhea will be controlled, so they will be able to move much more comfortably. For patients who cannot go out due to fear of not being able to control defecation, cannot go to the market or neighbors, TGFT and FMT are a very serious ray of hope.
Since the need for nocturnal defecation will be minimized with FMT or TGFT, chronic fatigue and depression symptoms will decrease along with better quality sleep.
Assoc. Prof. Dr. Murat KANLIÖZ
General Surgery Specialist
Table 1: Exclusion Criteria for Donor Selection in Total Gastrointestinal Flora Transplantation
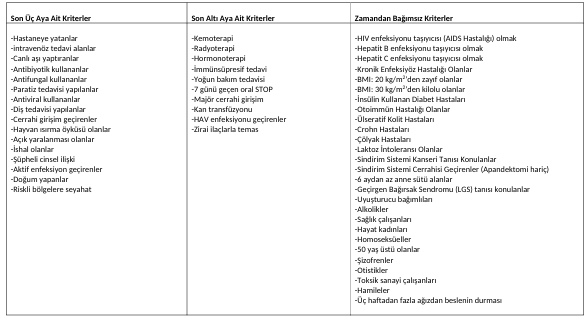
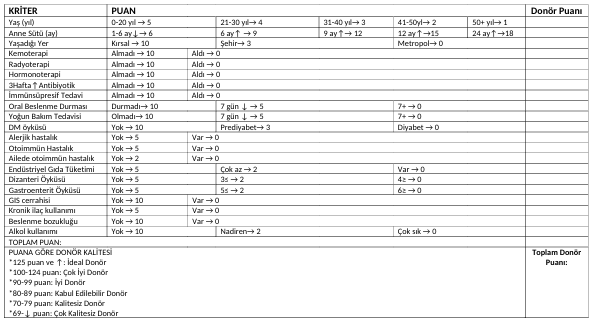
Table 2: Donor Quality Scoring